Home | About | About Autism
Page Disclaimer: This page contains numerous quoted sections and links to other websites, articles, and organizations managed, written, and led by autistic people. The intention of this page is to provide visitors with a starting point for learning more about autism. The best way to learn about autism is to listen to autistic people. Commonwealth Autism stands with the people we serve, so we use identity-first language (autistic, disabled) as an organization and respect autistic individuals who prefer person-first (has autism, has a disability).
What is Autism?
Autism is a developmental disability that affects how people experience the world around them. Autistic people are born autistic and will be autistic for their entire life. Due to myths and stereotyping of autistic characteristics, it’s more difficult for autistic adults, girls, nonbinary individuals, and people of color to receive a diagnosis. Anyone can be autistic, regardless of race, ethnicity, gender, or age.
Autism is not a spectrum in terms of a straight line, instead, it is a collection of traits, and different autistic people have different support needs in each area. Rebecca Burgess’ illustration offers a better understanding of the spectrum:

The Autistic Self Advocacy Network (ASAN) describes autism as:
“There is no one way to be autistic. Some autistic people can speak, and some autistic people need to communicate in other ways. Some autistic people also have intellectual disabilities, and some autistic people don’t. Some autistic people need a lot of help in their day-to-day lives, and some autistic people only need a little help. All of these people are autistic, because there is no right or wrong way to be autistic. All of us experience autism differently, but we all contribute to the world in meaningful ways. We all deserve understanding and acceptance.
Every autistic person experiences autism differently, but there are some things that many of us have in common.
- We think differently. We may have very strong interests in things other people don’t understand or seem to care about. We might be great problem-solvers, or pay close attention to detail. It might take us longer to think about things. We might have trouble with executive functioning, like figuring out how to start and finish a task, moving on to a new task, or making decisions.
Routines are important for many autistic people. It can be hard for us to deal with surprises or unexpected changes. When we get overwhelmed, we might not be able to process our thoughts, feelings, and surroundings, which can make us lose control of our body.
- We process our senses differently. We might be extra sensitive to things like bright lights or loud sounds. We might have trouble understanding what we hear or what our senses tell us. We might not notice if we are in pain or hungry. We might do the same movement over and over again. This is called “stimming,” and it helps us regulate our senses. For example, we might rock back and forth, play with our hands, or hum.
- We move differently. We might have trouble with fine motor skills or coordination. It can feel like our minds and bodies are disconnected. It can be hard for us to start or stop moving. Speech can be extra hard because it requires a lot of coordination. We might not be able to control how loud our voices are, or we might not be able to speak at all–even though we can understand what other people say.
- We communicate differently. We might talk using echolalia (repeating things we have heard before), or by scripting out what we want to say. Some autistic people use Augmentative and Alternative Communication (AAC) to communicate. For example, we may communicate by typing on a computer, spelling on a letter board, or pointing to pictures on an iPad. Some people may also communicate with behavior or the way we act. Not every autistic person can talk, but we all have important things to say.
- We socialize differently. Some of us might not understand or follow social rules that non-autistic people made up. We might be more direct than other people. Eye contact might make us uncomfortable. We might have a hard time controlling our body language or facial expressions, which can confuse non-autistic people or make it hard to socialize.
Some of us might not be able to guess how people feel. This doesn’t mean we don’t care how people feel! We just need people to tell us how they feel so we don’t have to guess. Some autistic people are extra sensitive to other people’s feelings.
- We might need help with daily living. It can take a lot of energy to live in a society built for non-autistic people. We may not have the energy to do some things in our daily lives. Or, parts of being autistic can make doing those things too hard. We may need help with things like cooking, doing our jobs, or going out. We might be able to do things on our own sometimes, but need help other times. We might need to take more breaks so we can recover our energy.
Not every autistic person will relate to all of these things. There are lots of different ways to be autistic. That is okay!”
Functioning labelings such as “high functioning” and “low functioning” should be avoided as they are vague and demeaning. ASAN summarizes the importance of functioning labels here.
“Functioning labels aren’t a good way to think about autism. We all have things we are good at and things we need help with. Using functioning labels makes it harder for us to get the help we need, and for us to make the choices we want. Instead, we should talk about people as individuals. Talk about what someone is good at, and what they need help with. This makes sure we can get what we need.”
Knowing early can make a significant difference.
Do you suspect you have an autistic child?
Find out for sure.
Early Signs of Autism
Children can be diagnosed as autistic when they’re young, some as early as 15 months. Not everyone is diagnosed early in life as it’s quite common for a child to not be diagnosed until they are older or even an adult, especially if they are a girl, a person of color, and/or do not have an accompanying learning disability.
Some of the main signs that a child may be on the autism spectrum include:
- Not drawing their parents’ or others’ attention to objects or events, for example not pointing at a toy or book, or at something that is happening nearby (or a child may eventually do this, but later than expected)
- Carrying out activities in a repetitive way, for example always playing the same game in the same way, or repeatedly lining up toys in a particular order
- Resistance to change or doing things differently
- Emerging difficulties with social interaction and social communication
- Behavior such as biting, pinching, kicking, pica (putting inedible items in the mouth), or self-injurious behavior
- Decreased babbling or use of language
You can learn more about typical developmental milestones on this timeline provided by the Centers for Disease Control and Prevention (CDC).
If you believe your child has autistic characteristics, contact your pediatrician, and they will make the appropriate referrals based on the findings of their initial assessment. Keep in mind some children learn to mask, so your doctor may not see what you see at home, where your child feels safe to unmask. If your doctor does not provide a referral and you still feel your child needs one, advocate for your child and seek a second opinion if possible.
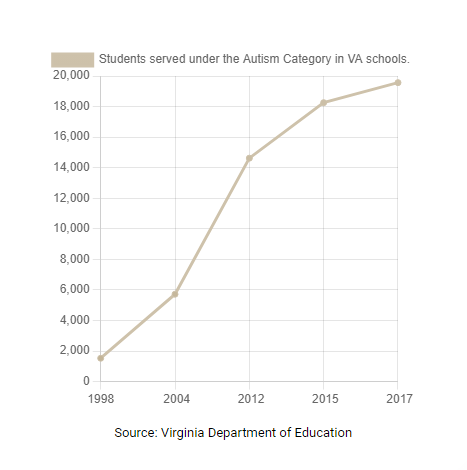
Prevalence
The CDC estimates that approximately 1 in 36 eight-year-old children have been identified as autistic. To learn more about the prevalence of autism by gender, geography, race/ethnicity, and more, take a look at the CDC’s Autism Data Visualization Tool.
- Among 8-year-old children, boys were nearly 4 times as likely as girls to be identified as autistic.
- 2020 marked the first time the Autism and Developmental Disabilities Monitoring (ADDM) Network found the percentage of girls identified as autistic to be over 1%.
- Also in 2020, Black, Hispanic, and Asian or Pacific Islander children had a higher percentage of autism than White children for the first time among 8-year-olds.
- Among 8-year-old children identified as autistic who had intelligence quotient (IQ) scores available, more than one-third (37.9%) also had an intellectual disability.
ASAN published a statement addressing the CDC’s latest ADDM Network report.
“ASAN is not surprised to see the diagnosis rate increase. We believe this increase reflects better recognition and diagnosis of autism across the U.S. We know that many disparities in diagnosis have become smaller. We know that children were evaluated earlier in some places and later in others, and believe that the differences in rates seen between different ADDM sites reflect that these disparities still exist. We expect that diagnosis rates will continue to rise as we work to address diagnostic disparities and improve access to diagnosis and support.”
Diagnosis
Although autism can be diagnosed as early as 15-18 months of age, the average age of diagnosis is about 4.5 years, and some people are not diagnosed until adulthood. More children who were born in 2016 (1.8%) received an autism diagnosis or special education classification by 4 years of age compared with children born in 2012 (1.1%), suggesting progress in early autism identification over time. In 2020, children born in 2016 (4-year-olds) were 1.6 times as likely as children born in 2012 (8-year-olds) to be identified as autistic by 48 months of age.
The following is ASAN’s statement regarding seeking an autism diagnosis as an adult:
“ASAN believes all autistic people are valid, whether or not we have a diagnosis. It can be really hard and expensive to get a diagnosis, especially for adults. Insurance usually does not cover getting an autism diagnosis as an adult. (For more information on why an autistic person might not get a diagnosis, see “Not all autistic people are diagnosed.”) We think more doctors need to be trained to give autism diagnoses, and insurance should cover getting a diagnosis. But doctors should also listen to autistic people when we talk about how our disability affects us, even if we don’t have an official diagnosis.”
Screening
The American Academy of Pediatrics recommends that all children be screened for autism at ages 18 and 24 months, along with regular developmental surveillance. If you are not sure whether your pediatrician screens for autism, ask. During a screening, the pediatrician observes the child’s behavior and development. The doctor may also ask the child’s caregiver to complete a questionnaire. If the doctor notices atypical or delayed development, they may recommend a comprehensive diagnostic assessment.
Once your doctor submits a referral, you may have to wait before you actually go for the assessment. In the meantime, your child could be referred to other teams such as speech therapy, occupational therapy, or education support services.
Medical Diagnosis
Various experts can make this diagnosis, including some psychologists, pediatricians, and neurologists. Psychologists are often involved in the diagnostic process. It is important that the expert making the diagnosis has extensive experience working with the wide range of characteristics associated with autism. The diagnostician should explain to you the reason for each test or assessment. You should be given plenty of time to ask questions. Don’t be afraid to ask for explanations or clarification if you need them.
To make a diagnosis of autism, diagnosticians draw on a number of sources of information:
- Patient interviews
- Observations in more than one setting
- Tests of cognitive and language abilities
- Medical tests to rule out other conditions
- Interviews with caregivers, teachers, or other adults who can answer questions about the patient’s social, emotional, and behavioral development
The current diagnostic criteria in the DSM-5 are not all-inclusive of autistic characteristics observed in girls, women, nonbinary people, people of color, and those who do not have an intellectual disability. Brian Reichow and Fred Volkmar discuss the narrowing of the autism diagnostic criteria in the DSM-5 here.
The Diagnostic Report
The diagnostician will tell you whether or not they think your child is autistic. They might do this on the day of the assessment (rarely), by phone on a later date, or in a written report that they send to you. Diagnostic reports can be difficult to read and understand in some places. You can call the diagnostician to talk through any parts of the report that you do not understand. Diagnostic reports are also very deficit-based, detailing what the child cannot do, which can be upsetting for caregivers to read.
The report should give a clear diagnosis. Phrases such as “has autistic tendencies” are not very helpful because they imply that a child is not autistic. This can cause problems when trying to access autism-specific support. It is very important to understand your child’s individual profile of needs. The report may say that your child presents a particular autism profile and may give recommendations for support.
Source: National Autistic Society
People may be told they show characteristics of a profile called Pathological Demand Avoidance (PDA); some self-advocates prefer it be called Pervasive Drive for Autonomy. PDA is not a formal diagnosis in the DSM-5. The PDA Society describes autistic demand avoidance as:
“Autistic people may avoid demands or situations that trigger anxiety or sensory overload, disrupt routines, involve transitioning from one activity to another, and activities/events that they don’t see the point of or have any interest in.
They may refuse, withdraw, ‘shutdown’ or escape in order to avoid these things.
Helpful approaches include addressing sensory issues, helping individuals adjust to new situations (for instance by using visuals or social stories), keeping to a predictable routine, giving plenty of notice about any changes or accepting that avoiding some things is perfectly acceptable.”
Educational Diagnosis
Just because your child receives a medical diagnosis of autism does not mean they will automatically receive the educational disability category of autism. This means your child may not be immediately eligible for special education services through the public school system. Contact your local school division’s special education department to request an assessment to obtain an educational diagnosis.
Individualized Education Program (IEP) meetings can be very intimidating for caregivers and for autistic students. Students often feel like the IEP meeting is a time when teachers and other professionals will only mention the things the student needs to improve upon, instead of the things that the student is doing well. Far too often, IEP meetings are led from a deficit-based approach instead of a strengths-based one. Rachel Dorsey, Hilary Crow, and Caroline Gaddy share the importance of valuing autistic attributes in this ASHA LeaderLive article.
Caregivers may want to seek the assistance of a Special Education Advocate to ensure their child is receiving the educational services they are entitled to. Lisa Wright, an IEP Special Education Coach, shares free IEP tips and resources for caregivers on her social media.
Some caregivers of autistic children report that their child has “behavioral issues” at school. Oftentimes, a child “acts out” because they have no other way to communicate, need additional support in the classroom, or are experiencing distressing sensory overload. Caregivers may also see more “behavioral issues” at home, which often means their child feels safe to unmask and decompress at home. Talk to your child’s educational team about your concerns. Autism Level UP! provides free resources for caregivers and educators to use in the classroom, at home, or really anywhere for autistic students.
For more information, refer to A Parent’s Guide to Special Education from the Virginia Department of Education (VDOE) and the autism page on the VDOE’s website. ASAN has a comprehensive list of resources and information regarding your educational rights that can be found here.
Therapy & Additional Services
The best practice when it comes to autism is focusing on supporting autistic people to live good lives and advocate for themselves. Autistic children do not need therapy simply because they are autistic.
“ASAN does not support any one kind of therapy for autistic people. Different things will work better for different autistic people. The most important thing is that any therapy should help autistic people get what we want and need, not what other people think we need. Good therapies focus on helping us figure out our goals, and work with us to achieve them.”
There are numerous evidence-based therapies that can be helpful for autistic people, such as occupational therapy, speech therapy, physical therapy, Augmentative and Alternative Communication (AAC), Acceptance and Commitment Therapy (ACT), music therapy, play therapy, Cognitive Behavioral Therapy (CBT), and many more.
Applied Behavioral Analysis (ABA) is one of the most commonly implemented services for autistic children and often the first suggestion for caregivers. ABA seeks to understand, predict, and change behavior and is delivered in a variety of settings, including home, school, clinic, and other community settings. ABA is a controversial practice due to the profession’s previous use of negative reinforcement strategies and the correlation between those exposed to ABA practices and PTSD symptoms. Not all ABA therapists are the same, and there is a growing number of ABA therapists, even some autistic ABA therapists, who are actively trying to rebrand and reframe ABA. David Meer wrote an in-depth assessment of the available therapies for autism and explained the controversy surrounding ABA while offering strategies to improve the field:
“Autistic adults are speaking out against this form of therapy, something that you rarely encounter with other treatment modalities. I do not know of many other therapies that have received as much backlash, to the point it is being labeled as abuse and traumatic. Autistic adults are urging us to reconsider how we deliver therapeutic services and the potential long-term consequences. Opponents of applied behavior analysis suggest that it can lead to prompt dependence, individuals who are conditioned to obey without questioning, loss of intrinsic motivation, decrease in self-confidence, and learned helplessness. A growing concern is fear that this form of therapy will exacerbate exposure to violent crime and sexual assault. Further research is needed, but these concerns need to be explored and addressed.
It is equally important not to simply dismiss behavior analysis – it is too valuable a science to ignore. Many of the principles are derived from sound theory and years of empirical research. There is no questioning that operant conditioning is an effective means to change behavior. It is important for us to understand how the environment impacts our thoughts, mood, and behavior. We should understand how sensory input impacts us so we can be prepared. We should understand the impact of operants on our future behavior. Knowledge of these systems can empower us to manage ourselves in response to the world and seek out accommodations as needed.”
When seeking support for your child, ask “What specific needs does my child have?” to determine the best options for them.
The Importance of Early Intervention
When it comes to intervention, the sooner, the better. In fact, research shows that intervention is most effective in the preschool years when the brain is developing most rapidly. Eligibility for early intervention services is based on an evaluation of your child’s skills and abilities.
The Infant & Toddler Connection of Virginia is Virginia’s early intervention system for infants and toddlers (age 0-36 months) with disabilities and their families. Any infant or toddler in Virginia who isn’t developing as expected or who has a medical condition that can delay typical development is eligible to receive early intervention supports and services under Part C of the Individuals with Disabilities Education Act (IDEA).
Early intervention supports and services focus on increasing the child’s participation in family and community activities that are important to the family. In addition, supports and services focus on helping parents and other caregivers know how to find ways to help their children learn during everyday activities.
The Infant & Toddler Connection of Virginia’s supports and services are available to all eligible children and their families regardless of a family’s ability to pay.
What is Neurodiversity?
Nicole Baumer, MD, MEd and Julia Frueh, MD summarize the neurodiversity movement as:
“Neurodiversity describes the idea that people experience and interact with the world around them in many different ways; there is no one “right” way of thinking, learning, and behaving, and differences are not viewed as deficits.
The word neurodiversity refers to the diversity of all people, but it is often used in the context of autism spectrum disorder (ASD), as well as other neurological or developmental conditions such as ADHD or learning disabilities. The neurodiversity movement emerged during the 1990s, aiming to increase acceptance and inclusion of all people while embracing neurological differences. Through online platforms, more and more autistic people were able to connect and form a self-advocacy movement. At the same time, Judy Singer, an Australian sociologist, coined the term neurodiversity to promote equality and inclusion of “neurological minorities.” While it is primarily a social justice movement, neurodiversity research and education is increasingly important in how clinicians view and address certain disabilities and neurological conditions.”
For those new to the subject of neurodiversity, it might be confusing to know what the right words are to use when speaking about the subject.
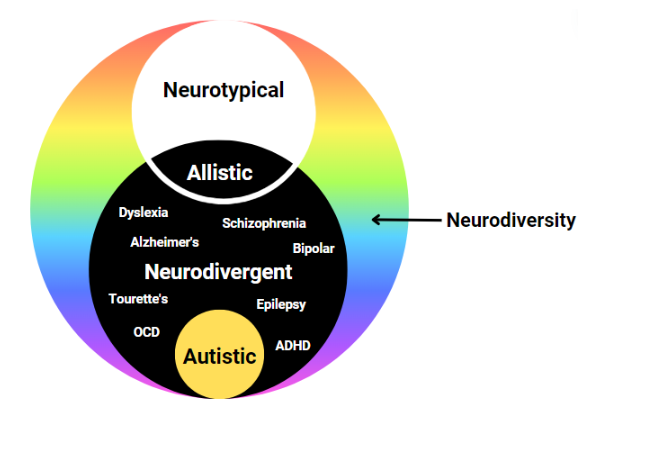
Neurodiversity: The natural diversity of human minds. It is a biological fact that we are diverse in our minds just like we are diverse in our ethnicity, gender, race, sexuality, etc.
Neurodivergent: An umbrella term for individuals who have a mind or brain that diverges from what is typical. It simply means having a mind that functions differently from what is considered the norm including learning, processing, interpreting, feeling, etc. Some examples of neurodivergencies include ADHD, autism, OCD, Alzheimer’s, dyslexia, bipolar, epilepsy, Tourette’s Syndrome, and many more.
Neurotypical: Having a mind or functioning that falls within society’s standards of what is deemed “typical”, “common”, or “normal”.
Neurodiverse: A term to describe a group of individuals who represent the spectrum of neurodiversity, which includes neurotypical and neurodivergent individuals. *Remember, an individual cannot be neurodiverse; however, one individual can be multiply neurodivergent (e.g. someone can be autistic and have OCD). Individuals who aren’t neurotypical would be neurodivergent.
Allistic: People who are not on the autism spectrum, which includes both neurotypical and non-autistic neurodivergent people
Autism Symbols
The rainbow infinity symbol represents neurodiversity; the full spectrum of colors represents the diversity of the autism spectrum as well as the greater neurodiversity movement. The gold infinity symbol has been adopted by the autistic community because the symbol for gold is AU and gold represents something of high value. There are new and evolving symbols created by autistic artists and activists, such as the colors of the rainbow weaving in motion created by Lori Shayew and Kelly Green. Most autistic people do not prefer the puzzle piece as the symbol of autism.
What is Masking?
Dr. Hannah Belcher is a lecturer, researcher, speaker, and author. Here Hannah discusses masking in autistic people, based on research and her own personal experience.
“To ‘mask’ or to ‘camouflage’ means to hide or disguise parts of oneself in order to better fit in with those around you. It is an unconscious strategy all humans develop whilst growing up in order to connect with those around us.
However, for us autistic folk the strategy is often much more ingrained and harmful to our wellbeing and health. Because our social norms are different to others around us, we often experience greater pressure to hide our true selves and to fit into that non-autistic culture. More often than not, we have to spend our entire lives hiding our traits and trying to fit in, even though the odds of appearing ‘non-autistic’ are against us.
Masking may involve suppressing certain behaviours we find soothing but that others think are ‘weird’, such as stimming or intense interests. It can also mean mimicking the behaviour of those around us, such as copying non-verbal behaviours, and developing complex social scripts to get by in social situations. With this comes a great need to be like others, and to avoid the prejudice and judgement that comes with being ‘different’.
Over time we may become more aware of our own masking, but it often begins as an unconscious response to social trauma before we even grasp our differences. I was 23 when I received my autism diagnosis, and it was only through learning more about masking that I realised how my diagnosis had been hidden for so long. It wasn’t that my autistic traits weren’t there, they’d just been in disguise for so long.
The strategy of masking shows just how clever and resourceful our young minds are at finding ways of coping. At some points in our lives, like during job interviews, it may have even be useful.”
Neurodiversity-Affirming Therapists
A neurodiversity-affirming therapist understands individual neurotypes have unique strengths, needs, and challenges and are not problems to be cured or solved. The neurodiversity movement shifts away from the medical model’s idea that neurodivergent people are “disordered.” Rachel Dorsey explains what strengths-based therapy really means here.
It can be difficult to find the right therapist whose values align with your own. This article from MACS PLLC provides a list of questions to ask a potential therapist to help determine if they are the right fit. There are neurodiversity-affirming therapist directories that can be found on Learn Play Thrive, Therapist Neurodiversity Collective, Inclusive Therapists, Neurodivergent Therapists, and Neurodivergent Practitioners Directory.
Avoiding Misinformation
It’s important to note that there is a lot of misinformation about autism on the internet and elsewhere. At best, this misinformation is confusing, and at worst, it can be harmful. We recommend the following resources to those interested in learning more about autism:
The Cost of Services
In Virginia, there are several ways to pay for services:
- Public funding: Early intervention, FAPE (Free Appropriate Public Education)
- Private insurance: As of January 2020, Virginia law mandates that state-regulated large group plans cover medically necessary care for autistic people, regardless of age
- Medicaid or a Medicaid Development Disability Waiver
- Commonwealth Coordinated Care Plus (CCC Plus) Waiver
- 529 ABLE (529A) accounts
- Out-of-pocket/private pay
Your Rights
Individuals with Disabilities Education Act (IDEA)
The Individuals with Disabilities Education Act (IDEA) is a federal law that ensures services to children with disabilities. IDEA governs how states and public agencies provide early intervention services (for ages birth to three) and special education and related services (for ages 3-21).
Free, Appropriate Public Education (FAPE)
Remember, just because your child has a medical diagnosis of autism does not mean they’ll automatically receive the educational disability category of autism. If your child does receive an educational diagnosis of autism, their Individualized Education Plan (IEP) team decides whether your local school division can provide FAPE. If it can’t, the state will pay for out-of-school placement. For more information regarding placement decisions, read A Parent’s Guide to Special Education from the Virginia Department of Education (VDOE).
Learn More from Autistic and Allistic Advocates
The following are listed in no particular order:
CA works with autistic people and their families to help them thrive. Every day, we’re building a future where the most vulnerable Virginians can actively participate in our community and realize their full potential.
Read our recent blog posts: